Introduction: Individuals living with sickle cell disease (SCD) have suffered from a lack of access to care, which is strongly associated with poor quality of care and negative health outcomes. The COVID-19 pandemic has likely further limited these patients' access to regular care. At the same time, the use of telehealth has rapidly expanded, which has been shown to improve access to care for many conditions. However, the pattern of adoption of telehealth among adult patients with SCD is little known. This study aimed 1) to examine the use of telehealth visits, along with in-person visits, among U.S. adults with SCD before and during the COVID-19 pandemic and 2) to identify patient subgroups that used a telehealth outpatient visit during the first year of the pandemic (03/2020-02/2021).
Methods: This retrospectivestudy used commercial insurance claims data from the Merative™ MarketScan ® Research Databases between 1/1/2019 and 12/31/2021. Individuals were included if they were between 18 and 62 years old, had ≥3 inpatient or outpatient claims with a SCD diagnosis, had no cancer diagnosis, and were enrolled in the data at least for 11 months each year of the study period. For the first objective, the number of telehealth and in-person outpatient visits made by the study population were measured each month throughout the study period. For the second objective, the outcome was whether or not a study individual used a telehealth visit during the first year of the pandemic (03/2020 to 02/2021) with any diagnoses. Demographic (age and gender) and socioeconomic (employment classification and status, geographic region, and rural vs. urban area) characteristics and baseline SCD-related outpatient visits 1-year prior (03/2019-02/2020) were measured and used as covariates when appropriate. Descriptive and multiple logistic regression analyses were performed. Employment classification and status were not included in the multiple logistic regression analysis due to a large number of other or unknown values.
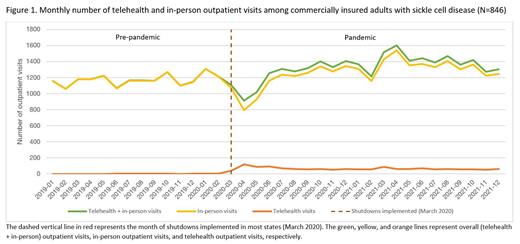
Results: Of the 846 SCD patients (mean [SD] age = 37.2 [12.8], 62.4% female) included, 342 (40.4%) used a telehealth visit during the pandemic. Before the shutdowns implemented in 03/2020, the mean number of outpatient visits was 1,172.4 [SD=69.9] per month; 1.1 [SD=1.2] (0.1%) were telehealth and 1,171.3 [SD=69.3] (99.9%) were in-person (Figure 1). During the first year of the pandemic (03/2020-02/2021), the mean outpatient visits were 1,243.3 [SD=154.7] per month; 67.7 [SD=22.2] (5.4%) were telehealth and 1,175.6 [SD=168.9] (94.6%) were in-person. After the first year, overall outpatient visits increased to 1,419.4 [SD=96.87] per month due to increases in in-person visits (1,357.1 [SD=92.0] per month) and a slightly decreased level of telehealth visits (62.3 [SD=10.3] per month). Patient characteristics associated with a higher likelihood of using telehealth include: age 35-44 (compared to 18-34; odds ratio [OR]: 1.466, 95% CI: 1.102-2.123, p=0.0433), female (compared to male; OR: 1.774, 95% CI: 1.321-2.399, p=0.0002), living in the West (compared to the South; OR: 1.887, 95% CI: 1.015-3.509, p=0.0448), and 13 or more outpatient visits 1 year prior to the pandemic (compared to 0-3 visits; OR: 1.722, 95% CI: 1.138-2.606, p=0.0101), whereas living in the North Central (compared to the South; OR: 0.538, 95% CI: 0.349-0.829, p=0.0050) or rural area (compared to urban; OR: 0.505, 95% CI: 0.336-0.759, p=0.0010) were associated with less likelihood of using telehealth, after controlling for other covariates.
Conclusion : Using nationally representative data, this study found that telehealth use among adults with SCD in the U.S. rapidly increased immediately after the shutdown orders in March 2020, decreased in a few months, and then remained steady afterwards. When a patient visit can be effectively conducted via telehealth, such as a follow-up visit for continued treatment, efforts focused on increasing telehealth use among young adults, males, those living in the North Central and/or rural areas could improve access to regular care, which could lead to better health outcomes.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal